#Healthcare Workflow
Explore tagged Tumblr posts
Text
A Day in the Life of a Medical Scribe: Behind the Scenes of Patient Documentation
Introduction
In the intricate tapestry of modern healthcare, there exists a role that often goes unnoticed by patients but is indispensable to the seamless functioning of medical practices – the medical scribe. As we peel back the layers of the healthcare workflow, we uncover the dynamic and crucial responsibilities of a medical scribe. This article offers an in-depth exploration of a typical day in the life of a medical scribe, shedding light on their role in patient documentation and the challenges they navigate.
The Morning Routine: Preparing for the Day Ahead
As the sun rises, a medical scribe steps into the bustling world of healthcare. The day starts with a review of the schedule, gaining insights into the patients who will be seen. Armed with knowledge of medical terminology, coding, and clinical procedures, the medical scribe is poised to provide valuable assistance to the physicians.
Patient Encounters: Charting the Journey
The heart of a medical scribe’s day revolves around patient encounters. As patients step into the clinic or hospital, the medical scribe is there, ready to capture every detail of the visit. This involves recording the patient’s medical history, current symptoms, and any relevant information. The scribe’s role is not only to document but also to actively listen, ensuring that no vital information is overlooked.
During the examination, the medical scribe is a silent observer, carefully documenting the physician’s findings. This real-time documentation not only allows the physician to focus on the patient but also ensures accurate and up-to-date electronic health records (EHRs).
Assisting the Physician: A Seamless Partnership
Medical scribes are the unsung heroes who enable healthcare providers to be fully present with their patients. By taking charge of documentation tasks, medical scribes allow physicians to engage in meaningful conversations, answer questions, and devise treatment plans without interruptions. This partnership between medical scribe and physician enhances patient-provider interactions, cultivating an atmosphere of trust and empathy.
Navigating Challenges: Precision and Adaptability
While the role of a medical scribe is rewarding, it also comes with its set of challenges. The fast-paced environment of healthcare demands precision, as any errors in documentation can have far-reaching consequences. Medical scribes must ensure that every detail is accurately recorded, from medications prescribed to diagnostic tests ordered.
Adaptability is another key trait of a medical scribe. Each patient brings a unique medical history and set of symptoms, requiring the scribe to swiftly adjust their documentation approach. The ability to maintain composure in high-pressure situations is essential.
Behind the Scenes: Post-Encounter Duties
After the flurry of patient encounters, the medical scribe’s work continues. They review and edit their documentation, ensuring clarity and correctness. This attention to detail is crucial for maintaining accurate medical records, which contribute to seamless care coordination among various healthcare professionals.
Conclusion: The Unseen Force in Healthcare Excellence
As the day winds down, it becomes evident that medical scribes are the gears that keep the healthcare machinery running smoothly. Their dedication to accurate and comprehensive documentation, along with their unwavering commitment to assisting healthcare providers, is the backbone of quality patient care.
The life of a medical scribe is a symphony of precise note-taking, active listening, and seamless collaboration. These professionals remain steadfastly behind the scenes, embodying the essence of teamwork and dedication. The next time you step into a healthcare facility, take a moment to appreciate the medical scribes, the silent champions who ensure that every patient’s journey is well-documented, and every healthcare provider’s efforts are fully supported.
0 notes
Text
How Healthcare Workflow Automation Safeguards Data and Streamlines Research
Let’s be realistic—healthcare these days is facing a whole lot of stress. Physicians, nurses, administrators, and scientists are doing more than ever before, and in the background, there's a gigantic heap of paperwork and data that has to be navigated with accuracy.
Caught in the midst of it all? A powerful tool that's quietly revolutionizing the practice of healthcare: healthcare workflow automation.
It's not merely about minimizing paper. It's about smarter, safer, and more secure healthcare—from clinics and hospitals to research laboratories. Let's discuss how automation is becoming the foundation of data security in research, compliance, and seamless healthcare operations.

1. From Paperwork to Peace of Mind: Why Automation Matters
If you've ever been in a hospital or clinic, you've likely seen how much time is spent on repetitive activities—patient forms, scheduling appointments, insurance authorization, and constant follow-ups. It's exhausting.
Here's where healthcare workflow automation comes in. It streamlines mundane tasks so doctors and healthcare workers can spend more time with patients and less time on paperwork.
Imagine this: rather than manually entering patient data into several systems, automation allows you to gather it once, process it in an instant, and safeguard it securely. All from appointment reminders to lab test results run smoothly—no bottlenecks, no errors.
The payoff? Speedier service, reduced burnout, and a streamlined healthcare experience.
2. Data Security Isn't Optional—It's Critical
We all know how precious health information is—and so do hackers, unfortunately. Whether it's individual health histories or clinical trials, healthcare information is a big-money target.
That's why today's healthcare systems are adopting healthcare data security solutions designed to address the threats of today.
Think encrypted storage, access controls based on roles, and detailed activity logs. A reliable healthcare document management system doesn’t just store your files—it protects them. And if a file’s ever changed or accessed? You’ll know exactly when, how, and by whom.
In a field where patient trust and research integrity matter more than anything, this level of security is no longer a luxury—it’s a necessity.
3. Compliance: The Unspoken Weight Healthcare Enforces
It's not easy keeping compliance with healthcare regulations. From HIPAA to GDPR to medical regulations in their own towns, the regulations are intricate, and they keep evolving.
Compliance for most organizations is like navigating a tightrope—one wrong move, and the fallout can be heavy.
This is where healthcare regulatory compliance software steps in to help shoulder the burden. By having the proper tools, you can make sure each document—whether patient file or research consent—is dealt with under the regulations.
Automated systems monitor changes, highlight errors, and even alert you to policy revisions. In audit time, rather than digging for paper, it's all a click or two away.
4. Research Deserves Better Protection
Research is the driving force behind healthcare. But behind every advancement is an ocean of sensitive information that must be treated with caution.
Whether you are handling clinical trial outcomes, lab results, or confidential procedures, research data security must be foolproof.
That's why research organizations are turning to secure healthcare document management systems that provide encrypted file sharing, restricted access controls, and safe backups.
This not only keeps your information secure—it also simplifies collaboration. Researchers from different departments (or even hemispheres) can collaborate without fearing leaks or breaches. That kind of reassurance is invaluable in the world of research.
5. The Big Picture: A Smarter, Safer Healthcare System
Collaborating all of this—automation, compliance, and security—produces a healthcare system that's not merely efficient, but durable.
A centralized healthcare document management system has it all under control and at your fingertips. No more running around for files across folders or departments. Everything you require, be it for treatment, billing, or research, is right in front of you—secure, searchable, and shareable.
It's not merely about time or error savings. It's about creating a healthcare system that can be trusted by patients and professionals.
Conclusion: Moving Healthcare Forward
We’re living in a time where information moves fast and expectations are even faster. Automation, when done right, isn’t about replacing people—it’s about empowering them.
With the right healthcare workflow automation, supported by strong healthcare data security solutions and dependable healthcare regulatory compliance software, every clinic, hospital, and research facility can move confidently into the future.
It's time to remove the burden from our teams, safeguard what is most important, and free up healthcare workers to do what they do best—care, heal, and innovate.
#healthcare workflow automation#healthcare data security solutions#healthcare regulatory compliance software#healthcare document management system#data security in research#research data security
0 notes
Text
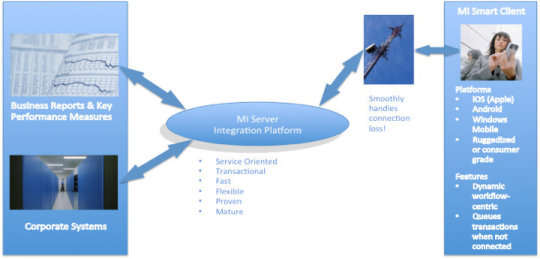
Driving EMR solutions value with adoption and change
Electronic Medical Record (EMR) systems can enhance the efficiency and performance of healthcare services by streamlining care workflows, promoting interdisciplinary working, and providing on-demand access to comprehensive patient information across healthcare teams.
EMR systems also provide a platform for more connected and patient-centric models of care across large geographies or populations, even though their impact in supporting this sort of care delivery reform has been limited to date.
Reported benefits of EMR solutions include improved patient safety, clinical outcomes, service efficiency, financial performance, and patient experience. These typically derive from improvements in care documentation, medication management, service insights and compliance, capacity and demand management, and patient communication, as well as reduced incidence of delayed or inappropriate care decisions.
However, achieving these benefits requires high levels of adoption by frontline staff and an ongoing program of value measurement and solution optimisation. Further, to realise value from technological advances like Artificial Intelligence (AI) and new service delivery models, EMR solutions must be architected with evolution and change in mind.
Realising value from EMR systems While much evidence supports the value of EMR systems, their implementation can be challenging, requiring well-executed change management involving meaningful and continued engagement with time-poor staff.
EMR deployments often focus on organisational value, typically detailed by a business case. Frontline staff often have to extrapolate meaning for their day-to-day working practices, which may or may not happen. Staff can be challenged by change without understanding its value to them as individuals, resulting in poor motivation and change management difficulties.
Articulating value in terms that resonate with frontline staff can help maintain momentum and enthusiasm for change. Established techniques from other industries, such as persona analysis, provide a helpful tool to express role-specific value definitions.
Collecting qualitative and quantitative data is also fundamental in evidencing and communicating the value of a EMR solution. It is good practice to plan and action this activity before going live. This establishes credible baseline data to compare against post go-live data to determine the value delivered and any unanticipated negative value for prioritisation in continuous improvement programs.
An ongoing journey, not an event The delivery and articulation of value is not an event but an ongoing journey. Post go-live analysis may focus upon a defined set of benefit and outcome measures, possibly described by the original business case. But an ongoing program of solution optimisation and value measurement helps to ensure the solution evolves with service needs, whilst identifying underperforming aspects that require corrective intervention.
An important post go-live dataset, commonly overlooked, relates to solution adoption and activity. This highlights areas of functionality and configuration that perform well or those requiring further interventions like user training or solution configuration changes. Automated adoption dashboards (see Figure 1) also provide dynamic insights.
EMRs must evolve to support new value All EMR solutions will continue to be shaped by technological innovation and changing healthcare demands. A solution’s long-term success will depend on quickly and cost-effectively supporting new value opportunities presented by advances in technology, science, and service delivery models.
AI and Machine Learning (ML), for example, present realistic and affordable options to enhance the quality and outcomes of care interventions. In fact, it is hard to imagine an enterprise-scale EMR solution without AI capabilities in two years’ time.
Generative AI solutions already help care professionals consolidate, synthesise, and summarise patient record data to improve the efficiency and precision of care planning and interventions. ML examples include predictive analysis, such as identifying patients at a higher risk of readmission, developing conditions, or unexpected deterioration.
Integrating interoperability standards, such as Fast Healthcare Interoperability Resources (FHIR), will also become crucial. These facilitate the sharing of structured, coded, and actionable patient information across health and social care services. This is particularly important in enhancing the efficiency and effectiveness of care transitions and collaborative decision-making across large geographies or populations.
Enterprise EMR solutions will also evolve to provide genomic capabilities relating to test orders and results and, importantly, pharmacogenomic decision support to guide and inform the correct and appropriate use of medications for each individual. This understanding, combined with EMR technology, has the potential to transform care outcomes on a scale similar to the introduction of antibiotics.
Transformation and new models of care The term ‘digital transformation’ is hard to escape. But what does this mean for healthcare services adopting an EMR solution?
Digital transformation represents an organisational re-wiring to create value for the organisation and its consumers via innovative business models. However, while many initiatives deliver modernised healthcare interventions – such as video consultations, virtual wards, healthcare apps, and AI technologies – these have been primarily used to enhance existing models of care.
Recognition of the need for new models of care that reflect the demands of modern societies is rapidly gaining pace. Current integrated care models rely on the ability of EMR platform technologies to support the seamless flow of information across healthcare services for the planning, management, allocation, and delivery of healthcare interventions
The transformation of healthcare to deliver genuinely patient-centric and joined-up care workflows will require significant service reforms and a paradigm shift. In particular, it will require moving away from the dominance of acute care. Working in interdisciplinary teams spanning care sectors will also be a significant change and challenge for healthcare professionals.
EMR solutions must provide a critical enabling and supportive role for the unimpeded flow of information across a healthcare region to inform the joined-up planning, management, allocation, and delivery of timely and appropriate care interventions.
Whilst the value currently delivered by EMR solutions is significant and important, the overwhelming value for a modern-day EMR system is in supporting the new and emerging models of care we so desperately need.
About the author Darren Jones is Country Manager, Australia and New Zealand at InterSystems, a creative data technology provider which delivers a unified foundation for next-generation applications for healthcare, finance, manufacturing and supply chain customers in more than 80 countries, and electronic medical record systems which support advanced data management in hospitals. Based in Melbourne, Jones leads the company’s operations in Australia and New Zealand and supports the success of InterSystems customers.
#EMR solutions#electronic medical records#healthcare digital transformation#change management in healthcare#real-time healthcare insights#hospital EMR adoption#clinical workflow optimization#staff adoption EMR#healthcare IT systems#hospital technology innovation#patient care improvement#EMR implementation strategies#healthcare data management#digital health solutions#hospital and healthcare journals
1 note
·
View note
Text
Top Sterile Processing Department Challenges Impacting Safety & Performance
Explore the biggest Sterile processing department challenges affecting healthcare facilities in Philadelphia. From Sterile processing training gaps to instrument sterilisation errors, discover how improper sterilisation processing can risk patient safety and hinder operational efficiency. Learn what hospitals and clinics in Philadelphia are doing to overcome these challenges and improve compliance, training, and quality standards in sterile services. This guide highlights real risks, consequences, and practical solutions for sterile processing professionals in the region. Whether you manage a central sterile unit or are involved in compliance, this insight is vital for maintaining top-tier patient care.
Related Tags :- Sterile processing department challenges in Philadelphia hospitals Sterile processing training programs in Philadelphia How to reduce instrument sterilisation errors in Philadelphia clinics
#Sterile processing department challenges in Philadelphia hospitals#Sterile processing training programs in Philadelphia#How to reduce instrument sterilisation errors in Philadelphia clinics#Sterilisation processing compliance issues in Philadelphia#Best practices for sterile processing in Philadelphia healthcare#Central sterile department training courses in Philadelphia#Common SPD mistakes in Philadelphia medical facilities#Preventing surgical instrument contamination in Philadelphia#Sterile processing technician challenges in Philadelphia#Improving sterilisation workflow in Philadelphia hospitals
0 notes
Text
Why AI-Driven Data Workflow Automation is a Game-Changer for Healthcare
The healthcare industry is one of the most complex and data-intensive sectors, dealing with vast amounts of patient records, medical imaging, research data, billing, and administrative processes. Historically, these workflows have been manually managed, leading to inefficiencies, errors, and delays in patient care. AI-driven data workflow automation is transforming healthcare by streamlining processes, enhancing accuracy, and improving overall patient outcomes. In this blog, we will explore how AI-powered automation is revolutionizing healthcare, its benefits, real-world applications, and what the future holds for this groundbreaking technology.
The Need for Automation in Healthcare
Healthcare systems globally are struggling with challenges such as:
Overwhelming administrative burdens
Rising operational costs
Increasing patient expectations for faster and more personalized care
The need for better compliance with regulations such as HIPAA and GDPR
Data silos between hospitals, clinics, and insurance providers
AI-driven workflow automation addresses these challenges by automating repetitive tasks, integrating data sources, and improving decision-making capabilities through predictive analytics.
Key Benefits of AI-Driven Workflow Automation in Healthcare
1. Improved Efficiency and Productivity
AI can automate tasks such as scheduling appointments, processing insurance claims, and managing electronic health records (EHR). This reduces the administrative workload on healthcare staff, allowing them to focus on patient care.
2. Enhanced Accuracy and Reduced Errors
Manual data entry and processing errors can lead to misdiagnoses, incorrect billing, and treatment delays. AI-driven automation minimizes these risks by ensuring accurate data input, processing, and analysis.
3. Faster and More Personalized Patient Care
AI-powered chatbots and virtual assistants can help patients book appointments, receive reminders, and get answers to medical inquiries. Machine learning algorithms analyze patient data to recommend personalized treatment plans.
4. Cost Reduction
By automating repetitive and time-consuming tasks, healthcare organizations can cut labor costs and reduce operational expenses, making medical care more affordable and efficient.
5. Better Compliance and Security
AI-driven solutions ensure that sensitive patient data is handled according to regulatory requirements. Automated workflows can track and report compliance issues in real time, reducing legal risks for healthcare providers.
Applications of AI-Driven Data Workflow Automation in Healthcare
1. Electronic Health Records (EHR) Management
AI-powered automation helps in data extraction, categorization, and updating patient records without human intervention. This ensures real-time access to accurate and up-to-date information for doctors and medical staff.
2. Medical Imaging and Diagnostics
AI-driven image recognition tools can quickly analyze X-rays, MRIs, and CT scans, assisting radiologists in detecting diseases like cancer, fractures, and neurological disorders with high accuracy.
3. Appointment Scheduling and Patient Engagement
AI-powered chatbots and virtual assistants can handle appointment scheduling, send reminders, and answer patient queries, reducing the burden on healthcare staff and improving patient satisfaction.
4. Billing and Insurance Claims Processing
Automation streamlines medical billing by detecting errors, verifying insurance claims, and ensuring compliance with coding standards, leading to faster reimbursements and fewer claim denials.
5. Predictive Analytics for Disease Prevention
Machine learning algorithms analyze patient history, lifestyle, and genetic factors to predict disease risks and recommend preventive measures, helping reduce hospital admissions and improving public health outcomes.
6. Clinical Trials and Research
AI accelerates clinical trials by automating data collection, patient recruitment, and analysis of medical research, leading to faster drug development and approvals.
7. Telemedicine and Remote Patient Monitoring
AI-powered automation enables remote patient monitoring through wearable devices that collect and analyze health data in real time, allowing doctors to intervene before conditions worsen.
Real-Life Case Studies in AI-Driven Healthcare Automation
Case Study 1: Mayo Clinic – AI for Early Disease Detection
The Mayo Clinic, a renowned medical research center, has integrated AI-driven automation into its workflow to enhance early disease detection. One notable example is its use of AI-powered imaging analysis to detect heart disease and certain types of cancer earlier than traditional methods. By leveraging machine learning algorithms, Mayo Clinic's AI systems analyze thousands of medical images to identify patterns that may indicate disease, helping doctors make more accurate diagnoses faster. This AI-driven approach has significantly reduced diagnostic errors and improved patient outcomes, demonstrating the power of AI in predictive medicine.
Case Study 2: Mount Sinai Health System – AI-Powered Radiology Workflow
Mount Sinai Health System in New York has implemented AI automation in its radiology department to streamline image analysis and reporting. The hospital's AI-driven workflow automates the sorting and prioritization of medical images, allowing radiologists to focus on the most urgent cases first. By analyzing CT scans, MRIs, and X-rays in real time, the AI system flags abnormalities such as tumors, fractures, and internal bleeding, expediting the diagnostic process. This has reduced patient wait times and improved treatment planning, showcasing how AI can enhance efficiency in high-demand medical environments.

Challenges and Considerations
Despite its advantages, AI-driven workflow automation in healthcare comes with challenges:
Data Privacy and Security: Ensuring that AI systems comply with HIPAA, GDPR, and other regulations is crucial to protecting patient data.
Integration with Legacy Systems: Many hospitals still use outdated systems that may not easily integrate with AI-powered solutions.
Trust and Adoption: Healthcare professionals may be skeptical of AI-based decision-making and need proper training to understand its benefits.
Cost of Implementation: While AI-driven automation leads to cost savings in the long run, the initial investment can be high for smaller healthcare providers.
The Future of AI-Driven Workflow Automation in Healthcare
The future of AI in healthcare looks promising, with advancements such as:
AI-powered robotics for surgeries and rehabilitation – Surgical robots are becoming more precise, allowing for minimally invasive procedures with faster recovery times. AI-driven robotic-assisted surgeries will enhance accuracy and reduce risks.
Natural Language Processing (NLP) for better doctor-patient communication – AI-powered NLP will improve how healthcare providers interact with patients, translating complex medical jargon into simple terms and enabling voice-driven medical documentation.
Blockchain for secure and decentralized patient data management – AI and blockchain will combine to ensure patient records are secure, tamper-proof, and easily accessible across healthcare institutions.
AI-driven drug discovery and personalized medicine – AI is accelerating drug development by analyzing vast datasets to identify potential treatments and tailoring medications to individual genetic profiles.
AI-integrated wearable technology for proactive healthcare – Smart wearables with AI capabilities will track vital signs, detect anomalies, and alert healthcare providers before health issues escalate.
AI-driven mental health support – AI-powered chatbots and virtual therapists will assist in detecting and managing mental health conditions, making mental healthcare more accessible.
AI in emergency and disaster response – AI will play a crucial role in detecting disease outbreaks, optimizing hospital responses, and assisting in large-scale disaster management efforts.
As AI continues to evolve, its impact on healthcare will only grow, making medical services more efficient, accurate, and accessible.
AI-driven data workflow automation is undeniably a game-changer for the healthcare industry. By improving efficiency, reducing costs, and enhancing patient care, AI is paving the way for a smarter, data-driven healthcare ecosystem. While challenges remain, ongoing advancements and regulatory compliance measures will ensure that AI-powered automation becomes a standard practice in healthcare. The integration of AI-driven automation is the future of modern healthcare.
Learn more about DataPeak:
#datapeak#factr#saas#technology#agentic ai#artificial intelligence#machine learning#ai#ai-driven business solutions#machine learning for workflow#ai solutions for data driven decision making#ai business tools#artificialintelligence#aiinnovation#digital trends#digital technology#digitaltools#datadrivendecisions#dataanalytics#data driven decision making#data analytics#workflowautomation#best ai tools for data pipeline automation#ai platform for business process automation#ai driven data workflow automation#healthcare#ai healthcare
0 notes
Text
Radiology Practices
Safe Radiology Practice for a safer world, safer health
On World Health Day 2022, WHO will focus global attention on urgent actions needed to keep humans and the planet healthy and foster a movement to create societies focused on well-being.
As per WHO estimates, more than 13 million deaths around the world each year can be attributed to avoidable environmental causes. This includes the climate crisis which is the single biggest health threat facing humanity. The climate crisis is also a health crisis.
On this occasion, Aster Medical Imaging focuses on the role of radiology in this crisis and the need to promote an environmentally sustainable radiology practice.
A 2021 study published in the Journal of Vascular and Interventional Radiology analyzed greenhouse gases generated by a hospital-based interventional radiology (IR) department in a typical five-day workweek. The researchers concluded that the practice of IR generates substantial greenhouse gas volumes, a majority of which come from energy used to maintain climate control in the IR suite. They found that more than half of the emissions that were generated by the climate control system, and ultimately about a quarter of the emissions produced during the entire study, were generated at night and on weekend hours when the IR suite is rarely in use. Read more here about Radiology Practices
#radiology#sustainability#healthcare#environment#wasteReduction#sustainablehealthcare#energyefficiency#greenimaging#ecofriendly#procurement#greenhealthcare#responsibleSourcing#digitalhealth#workflow#teleradiology#medicalimaging#medical care#medical imaging#ctscan#mri#ultrasound#aster
0 notes
Text
#EHR patient portal#Healthcare workflow automation#Patient engagement tools#Medical practice management#Telehealth integration#Appointment scheduling portal#Secure patient communication#Healthcare IT solutions#EMR integration#Medical records access#HIPAA-compliant portal
0 notes
Text
Multi-Purpose Telemetric I.V. Gowns: Enhancing Patient Care and Monitoring

Medical professionals now use Multi-purpose telemetric IV gowns for continuous patient monitoring as an innovative solution that enhances both patient care quality and comfort while enabling real-time monitoring capabilities. Specialized gowns equipped with telemetric functions enable easy intravenous (IV) treatment access, which makes them necessary for contemporary healthcare environments. Hospital gowns with IV access and telemetry pockets surpass traditional hospital gowns because their design includes features for continuous patient monitoring and IV line administration. Modern patient care benefits from telemetry pockets and sensor-friendly fabric that enables medical staff to track patient vital signs through monitoring devices while maintaining comfort for the patient. The gowns include carefully designed openings that will allow easy access to IV lines so healthcare providers do not need to remove the gown during treatment procedures. The main advantage of multi-purpose telemetric IV gowns is that they enhance the quality of care experienced by patients. The gowns offer comfort to long-term medical patients because they are made of soft, breathable, hypoallergenic materials. These garments with wrap-around or overlap designs ensure privacy while enabling quick medical staff access to examinations and interventions. Medical institutions obtain multiple advantages from these gowns because they improve workflow processes, minimize patient interruptions, and maintain optimal hygiene practices. These products exist in reusable and disposable versions to meet different needs throughout medical facilities, including intensive care units and outpatient areas. Healthcare institutions achieve improved patient safety while delivering accurate monitoring and maintaining patient dignity through the implementation of advanced patient-monitoring hospital gowns in their patient care practices.
#patient monitoring technology#hospital gown innovations#real-time vital sign tracking#medical wearables#smart hospital gowns#telemetry-enabled patient gowns#intravenous access clothing#healthcare workflow efficiency#patient-centered hospital apparel#infection control hospital gowns#ICU patient monitoring solutions#wearable health monitoring systems#advanced medical textiles#breathable hospital garments#hypoallergenic patient gowns
0 notes
Text
Applications of Robotic Process Automation in Healthcare
Robotic Process Automation (RPA) is transforming the healthcare sector by streamlining repetitive tasks. Key applications include patient data management, appointment scheduling, claims processing, and inventory tracking. By reducing human error and enhancing efficiency, RPA ensures better resource allocation and improved patient care. With expertise in healthcare automation, USM Business Systems stands out as the best mobile app development company, providing cutting-edge RPA solutions for healthcare businesses.
#Robotic process automation in healthcare#RPA applications in healthcare#Healthcare automation benefits#RPA for medical billing#Automation in patient management#RPA in healthcare operations#Healthcare efficiency with RPA#Robotic automation in hospitals#RPA in claims processing#RPA for healthcare workflows#AI and RPA in healthcare#Digital transformation in healthcare#RPA in patient data management#Automation for medical records#RPA in healthcare industry
0 notes
Text
HIPAA Automation: Simplify Compliance & Boost Security
HIPAA Automation uses technology to simplify compliance, reduce manual work and increase efficiency. With automated tools you can do self-audits, manage security policies, track risks and be continuously compliant with HIPAA regulations. This saves time and resources and minimizes human error that can lead to non-compliance. HIPAA compliant workflow automation lets healthcare providers simplify compliance and focus on patient care.

Why Do You Need HIPAA Automation?
Healthcare organizations handle huge amounts of patient data, manual compliance is a cumbersome and time consuming task. Automating HIPAA compliance with healthcare regulatory compliance software has many benefits:
Ensures Regulatory Compliance – Automation helps organizations follow HIPAA rules for patient data.
Enhances Risk Management – Automated tools streamline risk assessments and policy enforcement.
Reduces Data Breach Risks – Security automation minimizes vulnerabilities and protects sensitive information.
Keeps Up with Changing Regulations – Compliance requirements change and automation keeps up.
Improves Accuracy and Efficiency – Automation reduces human error and ensures consistency in enforcement.
Strengthens Healthcare Data Security – With healthcare data security solutions organizations can protect patient records from breaches and cyber threats.
Steps to Get Started with HIPAA Automation
Understand HIPAA: Before you start with automation, get familiar with HIPAA’s Security Rule, Privacy Rule and Breach Notification requirements. This knowledge is key to choosing the right healthcare regulatory compliance software.
Conduct a Compliance Risk Assessment: Identify compliance risks by evaluating your organization’s policies and procedures. A thorough risk assessment will uncover vulnerabilities and ensure your compliance program is aligned with regulatory requirements.
Choose the Right Automation Tool: Select an automation tool that integrates with your existing systems. Common tools are HIPAA compliant workflow automation, Identity and Access Management (IAM), Security Information and Event Management (SIEM) and policy management platforms. Comprehensive solutions like Sprinto can handle all aspects of HIPAA compliance automation.
Test the Automation Tool: Once you’ve selected a tool, integrate it into your system and test thoroughly to ensure it meets HIPAA standards and works.
Train Your Employees: Compliance is not just about software; employees need to be trained on HIPAA and automation tools. Proper training ensures staff members know their role in maintaining compliance.
Monitor and Continuously Evaluate: After automation, monitor its effectiveness, update policies as needed and be compliant with evolving HIPAA regulations. Regular assessments supported by healthcare data security solutions will help you identify areas for improvement and prevent potential violations.Bottomline HIPAA automation makes compliance easy by reducing manual work, reducing risks and being regulatory compliant.
Conclusion
HIPAA automation simplifies compliance by reducing manual efforts, minimizing risks, and ensuring regulatory adherence. By leveraging HIPAA compliant workflow automation and healthcare regulatory compliance software, healthcare organizations can enhance security, improve efficiency, and maintain long-term HIPAA compliance with ease.
#hipaa compliant workflow automation#healthcare data security solutions#healthcare regulatory compliance software#healthcare document management system hdms#Cloud document management solutions
0 notes
Text

Hospital & Healthcare Journals highlight how EMR solutions drive value through change management, real-time insights, and staff adoption for better care.
#EMR solutions#electronic medical records#healthcare digital transformation#change management in healthcare#real-time healthcare insights#hospital EMR adoption#clinical workflow optimization#staff adoption EMR#healthcare IT systems#hospital technology innovation#patient care improvement#EMR implementation strategies#healthcare data management#digital health solutions#hospital and healthcare journals
1 note
·
View note
Text
Effective paperwork management is crucial in the healthcare industry, ensuring that patient information is accurate and easily accessible. Training staff at healthcare business in Casper, Wyoming, can significantly improve how paperwork is handled. Providing staff with the right tools and resources allows them to become more efficient in managing documents, ultimately leading to better patient care. Regular training sessions can help employees stay updated on best practices and new technologies that streamline paperwork processes.
0 notes
Text
Enhance Productivity and Reduce Errors with Healthcare Workflow Automation Software!
Efficiency, accuracy, and high-quality care are more important than ever in the rapidly changing healthcare sector. The need for creative solutions has become evident as healthcare professionals deal with mounting patient loads, intricate regulatory requirements, and resource limitations. Software for Healthcare Workflow Automation is among the best solutions for these issues.
Countermind is excited to provide a complete, user-friendly Healthcare Workflow Automation Software that aims to reduce procedures, minimize administrative types, and enhance staff and patient satisfaction because we recognize how complicated healthcare operations can be. In this blog, we'll explore how workflow automation is changing the healthcare industry and how Countermind's solution has the potential to completely change how medical professionals give care.
What is Healthcare Workflow Automation Software?
The use of technology to automate and optimize standard clinical and administrative procedures in healthcare settings is known as healthcare workflow automation. Workflow automates repeated, manual processes that are at risk for mistakes and delays, such as patient intake, appointment scheduling, billing, and clinical reporting.
Healthcare firms can increase patient care while lowering operating costs, minimizing human error, and improving respect for industry standards by automating certain procedures.
Why is Automation of Healthcare Workflow Important?
Increased Productivity: Workflows in the healthcare industry can contain several departments and processes, each with a distinct set of responsibilities. Healthcare workers can give more of their time to patient care when administrative tasks are automated. Without human assistance, processes like insurance verification, patient check-ins, and appointment scheduling are completed quickly and accurately.
Better Accuracy and Fewer Errors: Manual methods make it easy to make mistakes, particularly in high-stress settings like clinics and hospitals. By drastically lowering the possibility of errors, automation guarantees the accuracy and consistency of patient data, billing information, and medical records.
Savings on expenses: Healthcare firms can reduce expenses by automating common administrative procedures. Operations are more cost-effective when there is less paperwork, fewer administrative mistakes, and improved departmental communication.
Enhanced Adherence: Maintaining compliance with constantly evolving healthcare rules is a never-ending task. By guaranteeing that important procedures are standardized, tracked, and recorded, workflow automation assists healthcare professionals in responding to regulatory regulations, billing codes, and laws such as HIPAA.
Quicker Reaction Times: Routine procedures like clinical reporting, appointment scheduling, and patient data entry have been sped up by automation. This results in quicker patient reply, quicker decision-making, and shorter wait times, all of which enhance the patient experience.
Conclusion
Healthcare organizations may concentrate on providing high-quality treatment while cutting expenses and raising patient happiness by automating routine chores. With Countermind's Healthcare Workflow Automation Software, explore the future of healthcare administration and see how it can change your business operations right now. With our Mass Vaccination Program software, we are dedicated to helping healthcare organizations run effective vaccination efforts.
#clinical workflow#clinical workflow in healthcare#mass vaccination program#clinical workflow solutions
1 note
·
View note
Text
youtube
#Steroid-induced hyperglycemia#allogeneic stem cell transplant#glucose monitoring#early detection#graft-versus-host disease#quality improvement#glycemic control#patient safety#standardized workflow#hyperglycemia management#steroid therapy#transplant recipients#glucose regulation#clinical protocols#diabetes care#healthcare intervention#transplant complications#patient outcomes#medical monitoring#transplant unit procedures.#Youtube
0 notes
Text
Savvy with Savica: Nurse Call Systems Get a Tech Upgrade in Australia
Gone are the days of clunky call buttons and endless hallways echoing with generic alarms. The world of nurse call systems in Australia is undergoing a digital revolution, and Savica is here to keep you informed! Let's explore some of the hottest trends:
1. Mobile Magic: Imagine nurses receiving alerts and patient information directly on their smartphones. This is the power of mobile nurse call systems, allowing for faster response times and improved communication.
2. Beyond the Button: Say hello to multi-functional call stations with features like voice communication, fall detection sensors, and even integration with patient monitoring systems. These advancements provide a more comprehensive picture of a patient's needs.
3. Interoperability is King: Modern systems seamlessly integrate with existing hospital infrastructure, including electronic health records (EHR). This streamlines workflows and eliminates data silos, leading to better patient care.
4. Safety First: Advanced nurse call systems can prioritize alerts based on urgency and even offer features like "wandering patient" detection for at-risk individuals. Safety is a top priority, and these systems are stepping up.
5. User-Friendly Focus: New systems are designed with user experience in mind, featuring intuitive interfaces and clear communication tools. This empowers both nurses and patients for a more positive hospital experience.
Savica keeps you smart about your space, and that includes healthcare facilities! These tech advancements in nurse call systems are transforming patient care in Australia. Stay tuned for future posts where we delve deeper into specific technologies and how they benefit hospitals and patients alike.
#savica#healthcare#hospitals#australia#nursecall#technology#innovation#mobilehealth#mobilealerts#patientcare#communication#workflow#safetyfirst#userexperience#aushealth#aushealthcare#australianhospital
1 note
·
View note